Epidemiology
Etiology
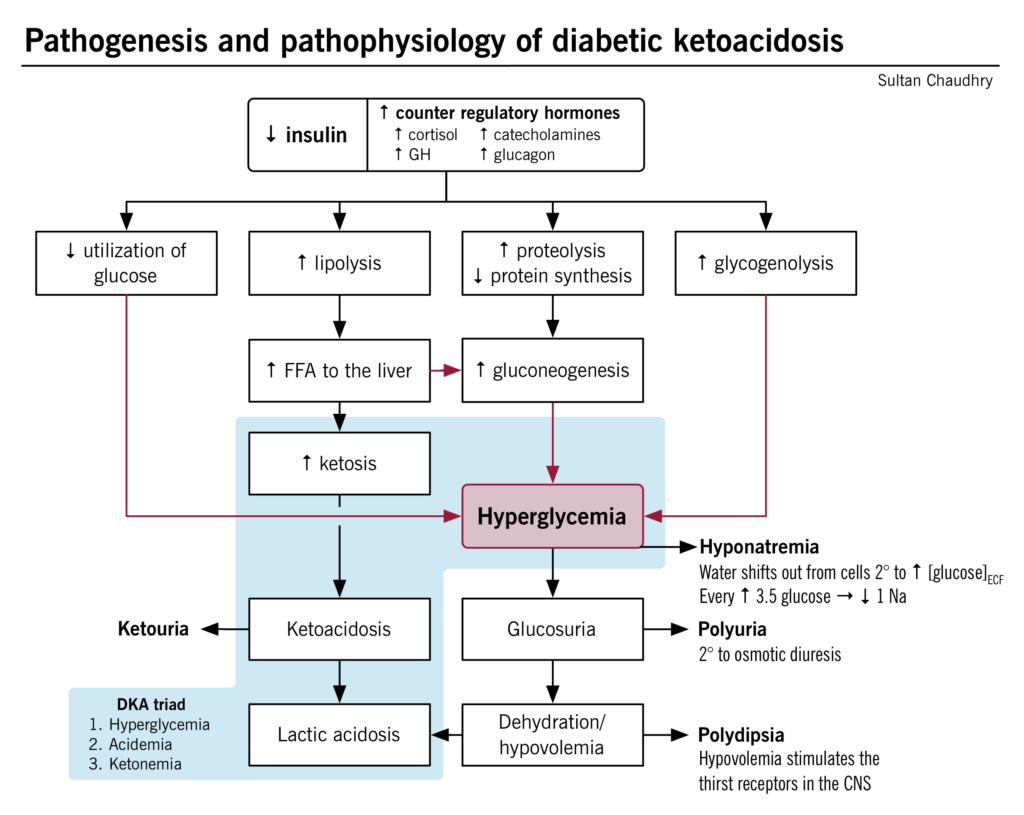
Pathophysiology
DKA
Intracellular potassium deficit
- As a result of hyperglycemic hyperosmolality, potassium shifts along with water from inside cells to the extracellular space and is lost in the urine.
- Insulin normally promotes cellular potassium uptake but is absent in DKA, compounding the problem.
- A total body potassium deficit develops in the body, although serum potassium may be normal or even paradoxically elevated.
- Insulin deficiency → hyperosmolality → K+ shift out of cells + lack of insulin to promote K+ uptake → intracellular K+ depleted → total body K+ deficit despite normal or even elevated serum K+
Tip
There is a total body potassium deficit in DKA. This becomes important during treatment, when insulin replacement leads to rapid potassium uptake by depleted cells and patients may require potassium replacement.
HHS
- Primarily affects patients with type 2 diabetes
- The pathophysiology of HHS is similar to that of DKA.
- However, in HHS, there are still small amounts of insulin being secreted by the pancreas, and this is sufficient to prevent DKA by suppressing lipolysis and, in turn, ketogenesis.
- HHS is characterized by symptoms of marked dehydration (and loss of electrolytes) due to the predominating hyperglycemia and osmotic diuresis.
Clinical features
Diagnostics
Tip
- DKA is the diagnosis in patients with type 1 diabetes who have hyperglycemia, ketonuria, and high anion gap metabolic acidosis with decreased bicarbonate!
- HHS is the diagnosis in patients with type 2 diabetes who have hyperglycemia and hyperosmolality!
Electrolytes and renal function
- Sodium:
- Hyponatremia is common in both DKA and HHS, due to hypovolemic hyponatremia and hypertonic hyponatremia
- Uncontrolled high blood sugar (hyperglycemia) in DKA acts like a magnet for water.
- This extra sugar in the blood pulls water out of cells, causing them to shrink.
- While the total body water stays the same, the concentration of sodium in the remaining extracellular fluid (outside the cells) gets diluted.
- Always check corrected sodium for hyperglycemia.
- Hyponatremia is common in both DKA and HHS, due to hypovolemic hyponatremia and hypertonic hyponatremia
- Potassium in DKA: normal or elevated (despite a total body deficit)
Treatment
- Fluid resuscitation: initially with isotonic saline (0.9% NaCl)
- Potassium repletion: for potassium level < 5.3 mEq/L
- Insulin therapy: initiate short-acting insulin once potassium level is > 3.3 mEq/L
- Identify and treat precipitating causes (e.g., sepsis).