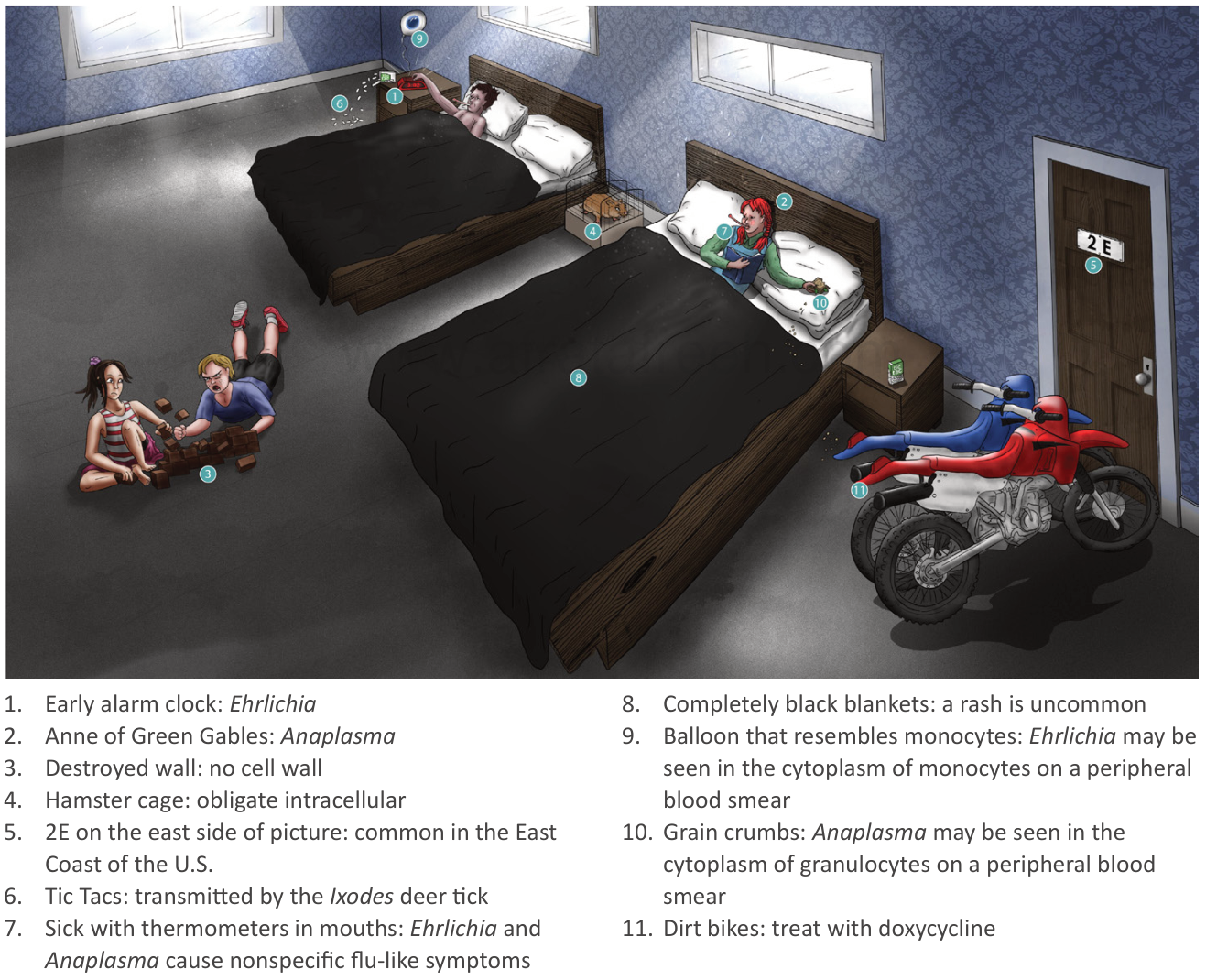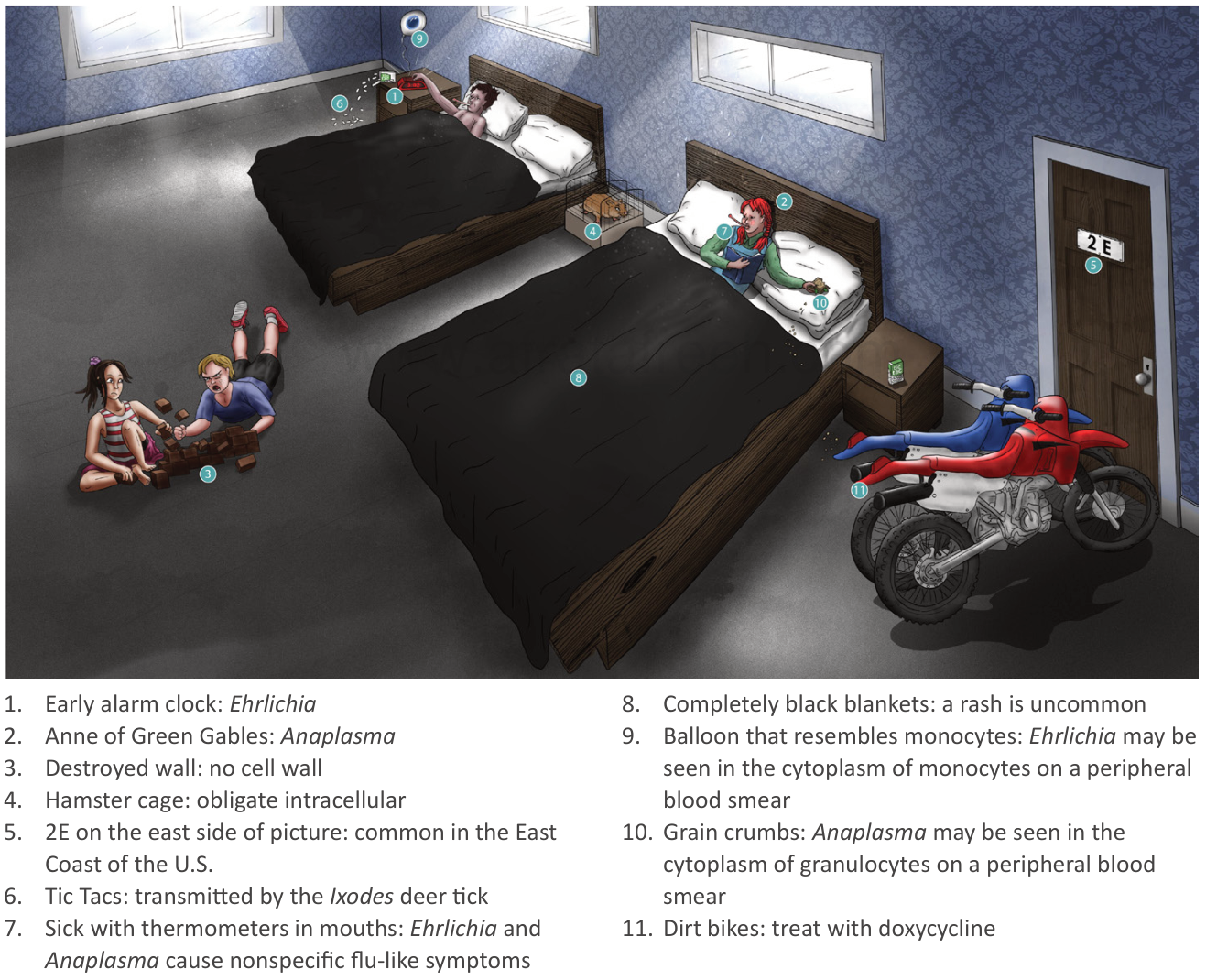
Ehrlichiosis
- Pathogens
- Vectors
- Lone star tick (Amblyomma americanum): E. chaffeensis and E. ewingii
- Deer tick (Ixodes scapularis): E. muris eauclairensis
- Distribution
- Mainly east of the Rocky Mountains
- Also some cases in the Southwest
- Clinical features
- Flu-like symptoms (e.g., fever, myalgia)
- Gastrointestinal symptoms (e.g., nausea, vomiting, abdominal pain)
- Hepatomegaly
- Rarely, symptoms of meningitis and/or encephalitis (e.g., headache, altered mental status, stiff neck, neurological deficits)
- Sometimes an erythematous maculopapular or petechial rash
- Adults: ∼ 30% of cases
- Children: ∼ 60% of cases
- Diagnostics
- Peripheral blood smear (with Wright stain or Giemsa stain): leukocytes with morulae (clustered inclusion bodies that resemble a mulberry)

- E. chaffeensis infection: morulae within monocytes
Tick paralysis
- Definition: a rare syndrome caused by the salivary neurotoxin of certain ticks, characterized by acute ataxia, that progresses to ascending paralysis
- Distribution: most commonly in the Rocky Mountains and northwestern US
- Pathophysiology
- Paralysis is caused by tick neurotoxin, which is produced in the tick’s salivary gland and introduced into the person’s blood.
- Clinical features
- Symptoms begin within 2–7 days of the initial tick bite.
- Typically starts with weakness in the lower extremities
- Escalates to ascending flaccid paralysis that progresses rapidly and can lead to respiratory failure due to respiratory muscle weakness
- Sensory deficits are usually absent.
- Cranial nerve palsies may occur (e.g., CN III palsy).
- No fever or rash
- Treatment
- Locate and remove the tick
- Removal of ticks usually results in improvement within 1 hour w/ recovery after several days