Etiology
- Primary ITP: idiopathic (most common)
- Secondary ITP associated with:
- Autoimmune disorders: SLE, Antiphospholipid syndrome
- Malignancy: lymphoma, leukemia (particularly CLL)
- Infection: HIV, HCV
- Drugs: e.g., quinine, beta-lactam antibiotics, carbamazepine, heparin, vaccines, linezolid, sulfonamides, vancomycin, TMP-SMX, antiepileptics
The acute form is typically seen in children after a viral disease.
Pathophysiology
Antiplatelet antibodies (mostly IgG directed against, e.g., GpIIb/IIIa, GpIb/IX) bind to surface proteins on platelets → sequestration by spleen and liver → ↓ platelet count → bone marrow megakaryocytes and platelet production increase in response (in most cases).
Clinical features
- Mostly asymptomatic. Splenomegaly is very unusual in ITP and makes other diagnoses more likely!
- Although platelets can undergo splenic sequestration in ITP, the primary mechanism responsible for the thrombocytopenia is immune destruction.
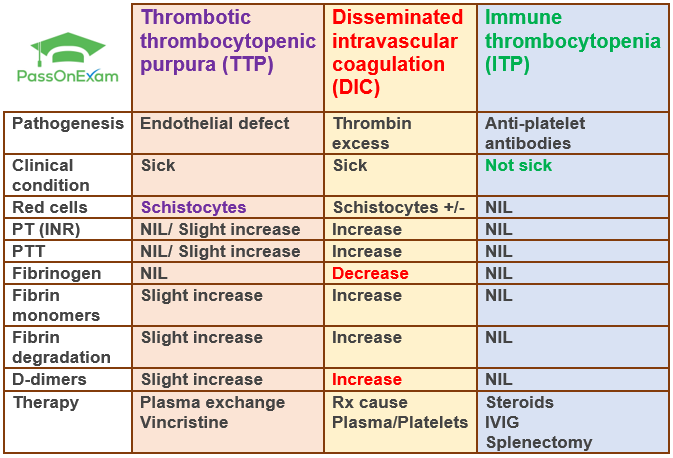
Differential diagnostics
| Feature | Thrombotic Thrombocytopenic Purpura (TTP) | Immune Thrombocytopenia (ITP) |
|---|---|---|
| Patho | ↓ ADAMTS13 activity → Large vWF multimers → microvascular platelet thrombi | Anti-platelet (anti-GpIIb/IIIa) Abs → splenic destruction of platelets |
| Presentation | Pentad (FAT RN): Fever, Anemia (MAHA), Thrombocytopenia, Renal failure, Neurologic sx (e.g., confusion, stroke). Often acutely ill. | Isolated mucocutaneous bleeding (petechiae, purpura, epistaxis). Often asymptomatic. No splenomegaly. |
| Labs | MAHA triad: Anemia, Thrombocytopenia, Schistocytes on smear. ↑LDH, ↑Bilirubin, ↓Haptoglobin. Normal PT/PTT. Dx confirmed by ADAMTS13 assay (<10%). | Isolated thrombocytopenia (<100,000/µL). Smear may show megathrombocytes. Otherwise normal CBC & smear. Normal PT/PTT. Dx of exclusion. |
| Tx | EMERGENT. Plasma exchange (PEX) is first-line & life-saving. Corticosteroids, Rituximab. Platelet transfusion is CONTRAINDICATED (fuels thrombosis). | 1st line: Corticosteroids, IVIG. 2nd line: Splenectomy, Rituximab, TPO-RAs (e.g., romiplostim). Observe if plt >30k & no bleeding. |