Epidemiology
Etiology
Most common causes
- Biliary pancreatitis (∼ 40% of cases; mostly caused by gallstones)
- Blockage of the common bile duct and pancreatic duct
- Alcohol-induced (∼ 20% of cases)
- Idiopathic (∼ 25% of cases)
Other causes
- Recent endoscopic retrograde cholangiopancreatography (ERCP) procedure
- Drugs (eg, azathioprine, sulfasalazine, furosemide, valproic acid)
- Infections (eg, mumps, Coxsackie virus, Mycoplasma pneumoniae)
- Hypertriglyceridemia: caused by severe hypertriglyceridemia (> 1,000 mg/dL) t
- Pathogenesis involves toxic fatty acids that are released from triglycerides via breakdown by pancreatic lipase. Associated with primary (e.g., type V hyperlipidemia) as well as secondary (e.g., due to medications) forms of hypertriglyceridemia.
- Structural abnormalities of the pancreatic duct (strictures, cancer, pancreas divisum) or of the ampullary region (choledochal cyst, stenosis of sphincter of Oddi)
- Surgery (particularly of the stomach and biliary tract and after cardiac surgery)
- Hypercalcemia
Pathophysiology
Clinical features
Symptoms
- Constant, severe epigastric pain
- Classically radiating towards the back
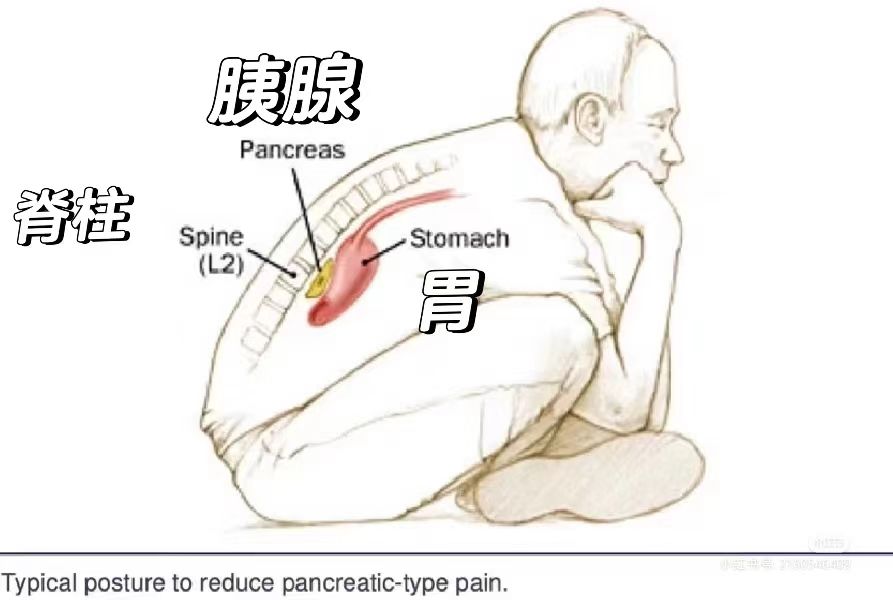
- Worse after meals and when supine
- Improves on leaning forwards
- Classically radiating towards the back
- Nausea, vomiting
- Fever
Examination findings
- General
- Signs of shock: tachycardia, hypotension, oliguria/anuria
- Due to distributive shock from cytokine release, and third-spacing of intravascular fluid.
- Abdominal examination
- Signs of shock: tachycardia, hypotension, oliguria/anuria
- Abdominal tenderness, distention, guarding
- Ileus with reduced bowel sounds and tympany on percussion
- Ascites
- Skin changes (rare)
- Cullen sign: periumbilical ecchymosis and discoloration (bluish-red)

- Grey Turner sign: flank ecchymosis with discoloration
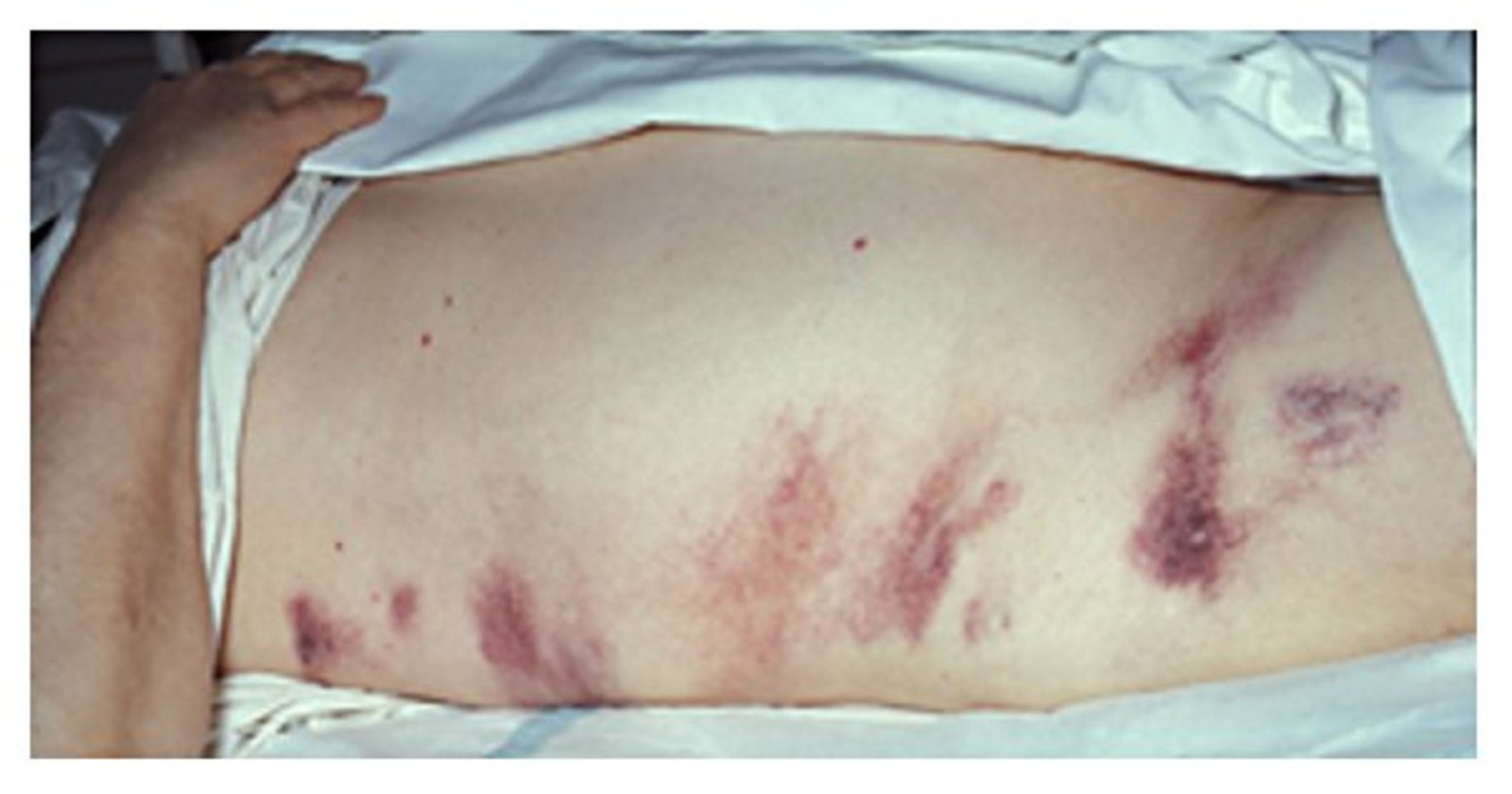
- Fox sign: ecchymosis over the inguinal ligament
- Cullen sign: periumbilical ecchymosis and discoloration (bluish-red)
Tip
Circulating pancreatic enzymes cause swelling of the subcutaneous tissue and localized hemorrhages. These signs, though nonspecific, suggest retroperitoneal bleeding and are associated with a poor prognosis.
- Pulmonary examination: signs of pleural effusion and/or ARDS may be present
- Pancreatitis is a major risk factor for ARDS as it results in the release of large amounts of inflammatory cytokines and pancreatic enzymes into the circulation, which leads to infiltration of neutrophils into the pulmonary interstitium and alveolar spaces.
Tip
As the pancreas is a retroperitoneal organ, abdominal guarding may not be present with the typical hard rigidity seen in inflammation of intraperitoneal organs. Instead, the abdomen is distended and elastic on palpation.
Diagnostics
- Diagnostic Criteria (Requires ≥2 of 3):
- Acute epigastric pain radiating to the back.
- Serum lipase (or amylase) ≥3x the upper limit of normal.
- Characteristic findings on imaging (e.g., CT, US).
- Key Labs:
- Lipase: Most specific and preferred test. Has a longer diagnostic window than amylase.
- Rises within 4-8 hours, peaks at 24 hours, and remains elevated for 8-14 days, providing a wider diagnostic window.
- Amylase: Less specific; can be elevated in other conditions.
- Rises within 6-12 hours and returns to normal more quickly (3-5 days).
- Important: The degree of enzyme elevation does NOT correlate with prognosis or severity.
- Lipase: Most specific and preferred test. Has a longer diagnostic window than amylase.
- Key Imaging:
- Imaging is NOT needed for diagnosis if clinical presentation and labs are classic.
- Ultrasound (US): First-line imaging to look for a biliary etiology (gallstones).
- Contrast-Enhanced CT (CECT): Gold standard for assessing complications (e.g., necrosis). Best performed >72 hours after symptom onset.
Tip
Lipase and amylase levels do not need to be trended once acute pancreatitis has been diagnosed, because levels do not correlate with prognosis or severity and do not impact management decisions.
Treatment
- Primary Goal: Supportive care is the cornerstone of management. There is no specific medication to stop the pancreatic inflammation itself. The goal is to prevent complications by supporting the patient through the acute phase.
- Early open surgery on an acutely inflamed pancreas significantly increases morbidity and mortality. The historical approach of immediate surgical debridement has been abandoned due to poor outcomes.
Key Interventions
- IV Fluids:
- Crucial first step. Moderately aggressive resuscitation is now favored.
- Lactated Ringer’s (LR) is the preferred fluid.
- Pain Control:
- IV opioids (e.g., Fentanyl, Hydromorphone).
- Nutritional Support:
- Mild AP: Start low-fat diet as soon as tolerated. NPO is outdated.
- Severe AP: Early enteral feeding (within 24-48h) is superior to TPN.
- Antibiotics:
- NOT for prophylaxis.
- Use only for confirmed infected necrosis or extrapancreatic infections (e.g., cholangitis).
- Monitoring:
- Watch O2, electrolytes, and calcium (risk of hypocalcemia).
Etiology-Specific Management
- Gallstones:
- Urgent ERCP if cholangitis is present.
- Cholecystectomy during the same hospital admission to prevent recurrence.
- Alcohol:
- Cessation is mandatory.
- Hypertriglyceridemia:
- Insulin infusion or apheresis in severe cases.
Complications Management
- Infected Necrosis:
- Antibiotics + Drainage. A “step-up” approach (percutaneous drain first, then endoscopic/surgical necrosectomy) is preferred.
- Pseudocyst:
- Drainage only if symptomatic, infected, or rapidly enlarging. Otherwise, observe.