Epidemiology
Etiology
Risk factors
- For contracting HPV infection
- Environmental risk factors
- Cigarette smoking and/or exposure to second-hand smoke (for squamous cell cancer types only)
- In-utero exposure to diethylstilbestrol (DES)
Pathophysiology
Overview of terminology
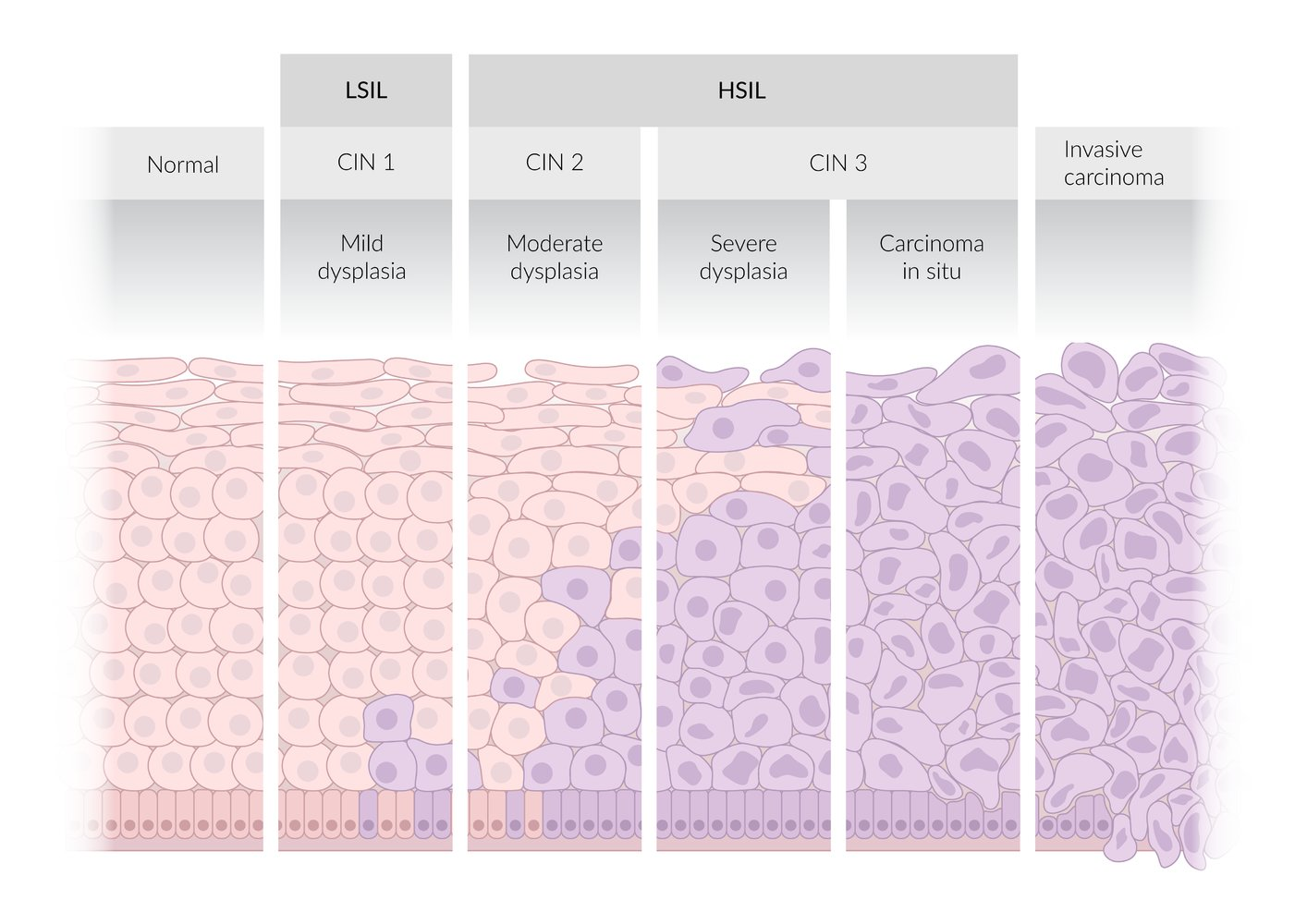
Two-tiered terminology (Bethesda system)
- High-grade squamous intraepithelial lesion (HSIL)
- Lesions with moderate to severe epithelial dysplasia that are most likely associated with persistent HPV infection
- HSIL lesions can progress to invasive cervical cancer (precancerous lesion).
- Low-grade squamous intraepithelial lesion (LSIL)
- Lesions with mild epithelial dysplasia that are typically associated with transient HPV infections
- Correlates with CIN1
Three-tiered terminology
- Cervical intraepithelial neoplasia (CIN) is characterized by epithelial dysplasia that begins at the basal layer of the squamocolumnar junction and extends outward.
- Based on the degree of dysplasia, lesions are classified as CIN1 (mild), CIN2 (moderate), or CIN3 (severe).
Current standard
The current standard for reporting cervical histopathology and cytopathology to ensure optimal management is a combination of the two-tier and three-tier system (i.e., the two-tiered nomenclature with an additional qualifier using the intraepithelial neoplasia nomenclature).
- LSIL correlates with CIN1.
- HSIL correlates with CIN3 and CIN2.
- HSIL should be specified as HSIL (CIN2), HSIL (CIN3), or HSIL unspecified.
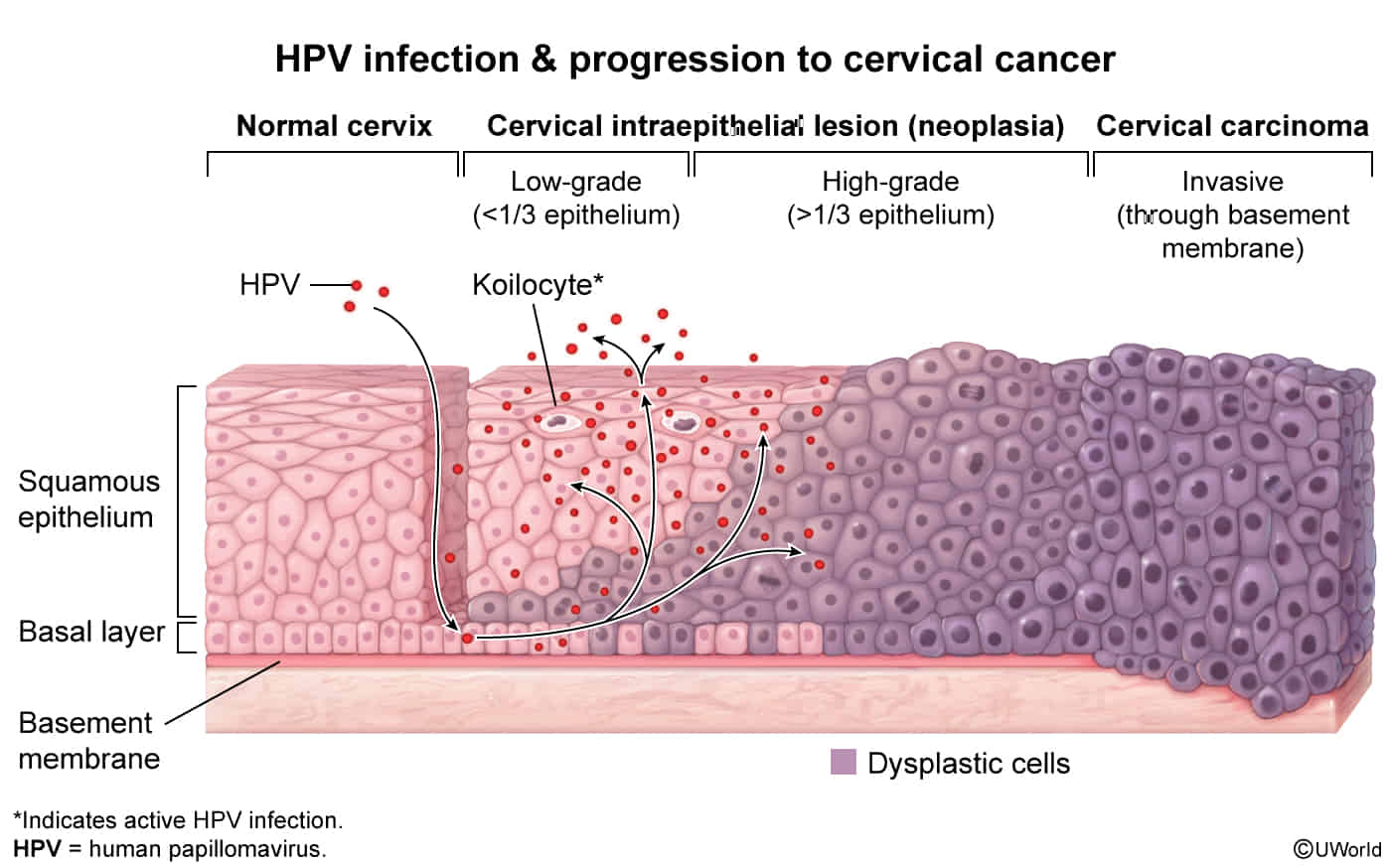
Normal cervix
- Endocervix: inner part of the cervix proximal to the uterine external os
- Composed of simple columnar epithelium with mucous-producing cells
- Cervical transformation zone: physiologic transition zone between the endocervix and ectocervix
- Exact location is variable
- Site of the squamocolumnar junction: the border between metaplastic squamous epithelium and simple columnar epithelium
- Cervical cancer most commonly occurs in this zone.
- Ectocervix: outer part of the cervix distal to the uterine external os
- Composed of stratified squamous epithelium (nonkeratinized)
Clinical features
Diagnostics
Pathology
- Invasive cervical carcinoma is characterized by invasion of the tumor beyond the basement membrane of the cervical epithelium.
- HSIL and invasive cervical carcinoma most commonly arise from metaplastic squamous cell epithelium in the cervical transformation zone
Squamous cell carcinoma (∼ 80% of cases)
- Subtypes include large cell keratinizing, large cell nonkeratinizing, and papillary squamous cell carcinoma.
- Irregular cell morphology
- Hyperchromatic cells with nonspherical nuclei, mitotic activity, and prominent nucleoli
- Loss of basal membrane