Placental abruption
The partial or complete separation of the placenta from the uterus prior to delivery; subsequent hemorrhage occurs from both maternal and fetal vessels.
Epidemiology
- Occurs most often in the third trimester
Etiology
- Vascular changes
- Hypertension (most common cause)
- Preeclampsia/eclampsia
- (Abdominal) trauma: e.g., car accidents, falls, intimate partner violence
- Twin pregnancy
- Sudden decrease in intrauterine pressure ; decompression of an overdistended uterus (e.g., ruptured membranes in polyhydramnios)
- Previous abruption, chorioamnionitis, short umbilical cord
- Maternal age: < 20 years and > 35 years
- Alcohol and cigarette consumption, cocaine use
Clinical features
- Maternal symptoms
- Sudden onset of continuous vaginal bleeding (revealed abruptio placentae)
- In up to 20% of cases, the hemorrhage is mainly retroplacental and vaginal bleeding does not occur (concealed abruptio placentae).

- Sudden onset of abdominal pain or back pain
- Uterine tenderness
- Fetal distress (60% of cases)
- Decelerations on fetal heart monitor
Placenta previa
Presence of the placenta in the lower uterine segment, which can lead to partial or full obstruction of the internal os; high risk of hemorrhage (rupture of placental vessels) and birth complications
Risk factors
- Maternal age > 35 years, multiparity, short intervals between pregnancies
- Previous curettage or cesarean delivery
- Previous placenta previa, previous/recurrent abortions
Classification

- Placenta previa: placenta either partially or completely covers the internal os
- Previously, this category included marginal previa (placenta reaching the internal os), partial previa (placenta partially covering the internal os), and complete previa (placenta completely covering the internal os); these terms have been excluded from the new classification.
- Low-lying placenta: lower edge of the placenta lies less than 2 cm from the internal cervical os
Clinical features
- Sudden, painless, bright red vaginal bleeding
- Usually occurs during the 3rd trimester (before rupture of the membranes)
- Initial bleeding episodes are often self-limited and recur during the onset of labor
- Soft, nontender uterus
- Usually no fetal distress
Vasa previa
Condition in which the fetal vessels are located in the membranes near the internal os of the cervix, putting them at risk of injury if the membranes rupture
Etiology
- Placental anomalies, such as:
- Velamentous umbilical cord insertion
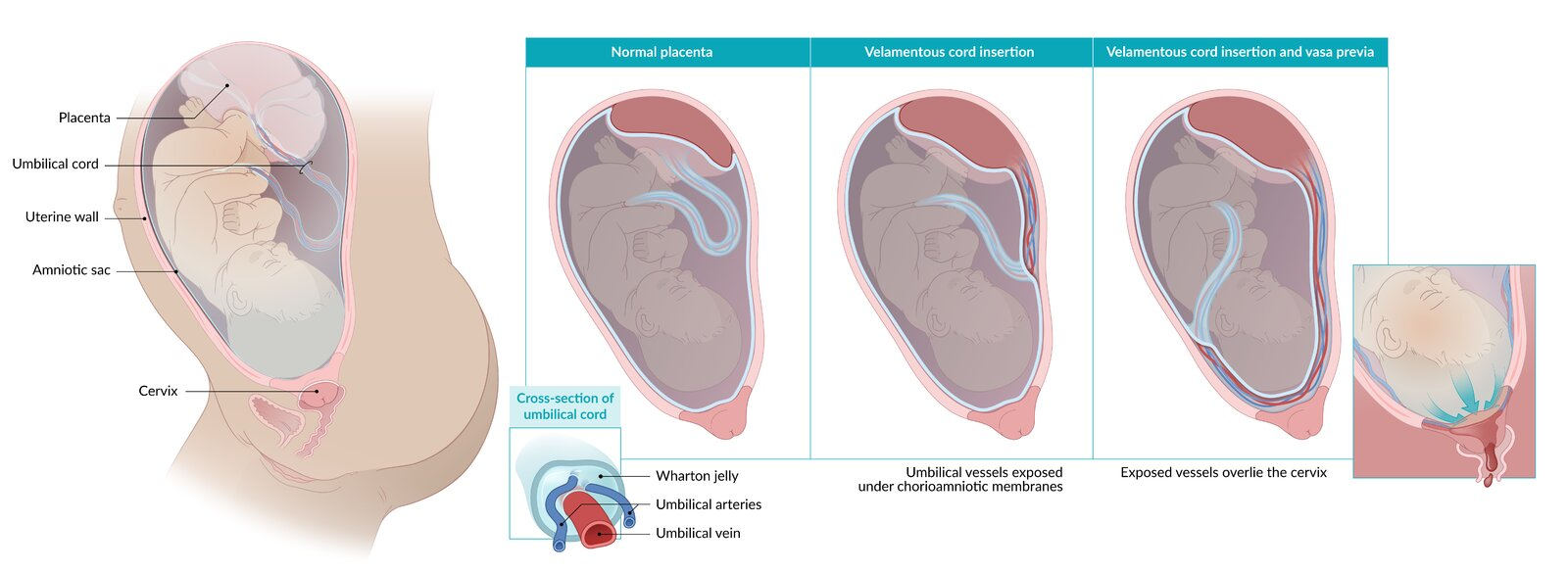
- Inserts in chorioamniotic membrane rather than placenta → fetal vessels travel to placenta unprotected by Wharton jelly
- Bilobate or succenturiate placenta
- Variation of the placental morphology with one or more accessory lobes developing separately from the main placental body
- Velamentous umbilical cord insertion
Clinical features
- Painless vaginal bleeding (fetal blood) that occurs suddenly after rupture of membranes
- Fetal distress (e.g., fetal bradycardia; decelerations or sinusoidal pattern on fetal heart tracings)
- Fetal death can occur quickly through exsanguination or asphyxiation if fetal vessels are compressed during labor.